
Part 1 of this article discussed olfactory tissue’s
remarkable regenerative potential and the efforts of various scientists
throughout the world to harness this potential by transplanti ng
it into the injury site of people with chronic spinal cord injury (SCI).
Part 2 discusses the pioneering work of one of these scientists,
Portugal’s Carlos Lima.
ng
it into the injury site of people with chronic spinal cord injury (SCI).
Part 2 discusses the pioneering work of one of these scientists,
Portugal’s Carlos Lima.
Olfactory Tissue:
Olfactory tissue, which covers about one-inch of the
upper nasal cavity, contains many cells with regenerative potential,
including renewable neurons, progenitor stem cells, and remyelinating
olfactory ensheathing cells (OECs). Olfactory neurons are comfortable
residing in the central and peripheral nervous system; because they
are the body’s only surface neurons, they readily regenerate from a pool
of progenitor stem cells. In addition, OECs can produce insulating myelin
sheaths around both growing and damaged spinal cord axons, secrete various
neuronal growth factors, and produce structural and matrix macromolecules
that lay the tracks for axonal elongation.
Carlos Lima:
A 48-year old
neuropathologist at Lisbon’s Egaz Moniz Hospital, Lima obtained medical
training in Portugal and Germany. In addition to olfactory-tissue
physiology, he is an authority on the neuropathology of HIV infection and
brain disorders similar to mad-cow disease.
Lima seemed
destined to work on olfactory processes. For example, before he was a
medical student, Lima was a rock-and-roll singer, and, with prescient
foresight, composed “Nose, Nose, Nose,” a song based
on a poem written by eighteenth century Portuguese Poet Manuel Bocage.
Lima’s guitar
still stands out among home-office computer equipment, and it was only the
pleading of his exam-studying son that prevented Lima from giving an
impromptu rendition of the song during my visit with him. The incident
reminded me again that scientific inspiration reflects the soul’s
creativity just as much as the mind’s intellect.
Lima’s scientific
epiphany came 15 years ago when, after reading about olfactory tissue’s
unique neurological properties, he immediately envisioned its potential
for bridging injured spinal cords. Since then, he has unwaveringly
directed his research toward this goal, carrying out extensive studies in
animals as well as human cadavers.
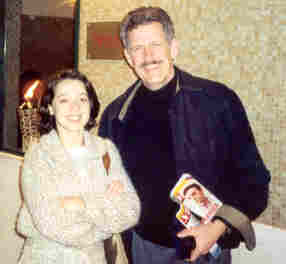
Lima emphasizes
that the project is a multidisciplinary collaboration that also includes
Pedro Escada, an ear-nose-and- throat
specialist who collects the patient’s olfactory tissue, Pratas Vital or
Hasse Ferreira, neurosurgeons who implant this tissue into the patient’s
spinal cord, and other Egaz Moniz Hospital specialists (Photo: Escada,
Vital, Ferreira & Lima).
throat
specialist who collects the patient’s olfactory tissue, Pratas Vital or
Hasse Ferreira, neurosurgeons who implant this tissue into the patient’s
spinal cord, and other Egaz Moniz Hospital specialists (Photo: Escada,
Vital, Ferreira & Lima).
Possessing a
panoramic vista of the Tejo River estuary, the Egaz Moniz Hospital has a
historical association with neurological innovation, including being named
after a 1949 Portuguese Nobel Laureate, who developed cerebral angiography
for visualizing brain blood vessels.
Patients:
Based on Lima’s
extensive preliminary research, the hospital’s ethics committee approved
the human clinical trials. Patients were subjected to various
neurological, neurophysiological (i.e., neuronal conduction), magnetic
resonance imaging (MRI), bladder-functioning, and psychological
assessments before and after treatment.
Assessments
included the “gold-standard” ASIA (American Spinal Injury Association)
impairment scales for measuring SCI-related sensory and motor impairment.
With these scales, patient improvement due to a specific intervention can
be assessed in a consistent fashion and more readily compared to other
studies. Patients were excluded if they had psychological disturbances,
multiple spinal cord lesions, confounding medical conditions, arm or leg
denervation, or severe spinal cord atrophy.
From July 2001 to
the beginning of 2003, Lima’s team has operated on four female and three
male patients. Three were quadriplegics and four paraplegics. Six of the
seven had ASIA-classified complete injuries. Ages ranged from 11-32
(averaging 22), and the time between injury and surgery varied from ½ - 6
½ years. Spinal cord lesions ranged from 1-6 cm (1 cm = .39 inches) in
length, although Lima now believes that the lesion optimally should be
less than 2-3 cm. Most injuries were contusion injuries, similar to those
sustained in car accidents.
Surgery:
The surgery
consists of harvesting olfactory tissue from the patient’s nasal cavity,
preparing it, and implanting it back into his or her spinal cord injury
site. The procedure takes 4-6 hours depending upon injury level and extent
of injury, presence of fixation plates or screws, etc. The patient is
discharged from the hospital after 4-7 days.
The critical
procedure is the collection of about one fourth of the patient ’s
olfactory tissue through unique procedures that maximize the harvesting of
that tissue and minimize the collection of closely associated nasal
respiratory tissue. Although Lima’s experience indicates that small
amounts of contaminating respiratory tissue are innocuous, it nevertheless
lacks olfactory tissue’s regenerative components. Because olfactory tissue
can diminish over time, patient age is important.
’s
olfactory tissue through unique procedures that maximize the harvesting of
that tissue and minimize the collection of closely associated nasal
respiratory tissue. Although Lima’s experience indicates that small
amounts of contaminating respiratory tissue are innocuous, it nevertheless
lacks olfactory tissue’s regenerative components. Because olfactory tissue
can diminish over time, patient age is important.
In contrast to other researchers who have started to
implant isolated OECs into patients with SCI, Lima uses whole olfactory
tissue for transplantation without attempting to separate cellular
components. He believes that more than one cell type is needed to maximize
regeneration in the injured cord, including, in addition to OECs, neurons
in different developmental stages, and precursor stem cells.
Because the graft
is taken from the patient,
immunosuppressive drugs are not needed to avert tissue rejection. In
addition, patients regain smelling ability within several weeks.
The neurosurgeon
exposes the cord’s injury site with a laminectomy and then myelotomy
(cutting open the cord’s membrane coverings). Although it is impossible to
remove all of the scar tissue at the injury site cavity, the scar’s top
and bottom stumps are taken off so that the cord is visible, and in
between, holes are made in the scar.
As the cavity is
being prepared, Lima dissects the isolated olfactory tissue into 20-30
pieces while it is immersed in a small amount of the patient’s
cerebrospinal fluid. The pieces are then implanted into the cavity. Lima
estimates that a 1 cm2 cavity filled by this tissue will
contain approximately 400,000 stem cells and 4 million each of mature
neurons, immature neurons, and other supporting cells.
Outcomes:
Although
preliminary results are promising, Lima emphasizes that much follow-up
work is needed to document long-term benefits and any delayed side
effects. Because only a short-time period has ensued since surgery for
many patients, benefits associated with neurological regeneration are not
expected to fully accrue for some time. Although Lima underscores that
patients should have realistic expectations and not anticipate an
all-encompassing, restoration-of-function panacea, he believes that even
modest restored function can have profound quality-of-life benefits.
Using the ASIA
standards, six of the seven patients regained some sensation and muscle
control within a month of surgery. Because the seventh patient had a
second undetected lesion, he did not improve.
Lima suggests
that this initial recovery may be due to bridging and remyelination of
available axons and also perhaps due to some post-surgical cord
decompression. Improvement should gradually continue with time as neurons
or their axons further regenerate and grow (~ 0.1 cm/day), remyelinate,
and make new connections.
This gradual
improvement is demonstrated by Lima’s first patient, a 21-year old female
who sustained a C7-T1 contusion-type injury six months before surgery. She
regained some sensory recovery about one month after surgery, voluntary
abdominal muscle control at two months, some gluteus and leg adductor
muscle control, including standing without leg braces after about nine
months, and recently some bladder control.
Overall, MRIs
indicate substantial filling of and continuity in the lesions by the
grafts, and electrophysiological assessments document voluntary muscle
control.
Lima’s patients
have had access to only modest post-surgical rehabilitation. He believes
maximal restored function will require much more aggressive
rehabilitation.
What Patients Say:
Luís, 29, sustained a 4-cm-long,
clinically complete, T4-5 injury two years ago while helping a friend
paint walls.
 After
misplacing a foot, his life turned upside down. When a friend told him
about Dr. Lima’s work, he immediately volunteered to be a candidate.
After
misplacing a foot, his life turned upside down. When a friend told him
about Dr. Lima’s work, he immediately volunteered to be a candidate.
“There was much uncertainty, but I
had nothing to loose,” he remembers.
Luís started noticing improvements
two or three weeks after his August operation. He first regained
sensitivity immediately below the injury site. Then came control of
abdominal muscles and recently abductor muscles, essential for equilibrium
when standing.
“Now I can feel the cold, and even
get goose pimples. Day by day, I rediscover my capacities,” he says
smiling broadly with a big smile. “And to accomplish it, I am ready to do
whatever it takes.”
Florbela, 32, sustained a
2-cm-long, C6 injury in a car accident six years ago. Her restored
function demonstrates the procedure’s potential for those with more
long-term injuries.
 Specifically,
within several months of her surgery, she recovered abdominal muscle
control, left-leg sensitivity, and, most recently, some grasping ability,
which occurred at home with her husband. She enthusiastically notes “We
have recorded everything with the digital camera; I want everybody to see
it”.
Specifically,
within several months of her surgery, she recovered abdominal muscle
control, left-leg sensitivity, and, most recently, some grasping ability,
which occurred at home with her husband. She enthusiastically notes “We
have recorded everything with the digital camera; I want everybody to see
it”.
American Patients:
At the time this
article was written, two American women with C6 injuries from 2001 auto
accidents were being scheduled for olfactory-tissue transplantation. They
are considered superb candidates due to their youth, excellent physical
health, and commitment to rigorous rehabilitation.
To help
disseminate this function-restoring surgery, Lima is attempting to develop
a collaboration with an U.S. hospital, in which Americans will travel to
Portugal for olfactory-tissue transplantation, and Portuguese patients
will travel to America for rehabilitation.
Conclusion:
At a 1995 congressional reception focused on SCI, a
colleague with high-level quadriplegia characterized the state of SCI
research by paraphrasing a famous Martin Luther King speech. He believed
that after a long trek in the wilderness, we have climbed the mountain and
for the first time can see in the distance the Promised Land of restored
function; some may complete the journey, and some may not.
Times have changed. This Promised Land is no longer a
mere vision hovering on the horizon. With groundbreaking physicians and
scientists guiding the way, the first pioneers with SCI are beginning to
step, in some cases literally, into this Land. Whether it is someone like
Luís and Florbela mentioned above, the Shanghai
motorcycle driver Huocheng who can now walk and control bladder and bowel
function because of a nerve-transfer surgery (PN, April 2002),
actor Christopher Reeve, who through innovative rehabilitation therapy can
now initiate never-expected movements (TIME, September 23, 2002),
or world pole-vault record holder Brian Sternberg who regained
considerable life enhancing function decades after injury through omental
transposition (PN, March 2001), an increasing number of such
pioneers are in the future. It is a growing reality coalescing in bits and
pieces, including the first olfactory-tissue transplantation carried out
by Dr. Carlos Lima’s team.
Acknowledgements:
The author is grateful for photos provided by
“Visão,” magazine, assistance provided by PN magazine and SERONO
Biotech, Portugal, and the liaison efforts of James Kelly, Texas.
About the Authors:
The authors are Laurance Johnston
and Sara Sá, a journalist for Visão, Portugal’s national news
magazine.
Adapted from article appearing in Paraplegia News, March, 2003 (For subscriptions, contact www.pn-magazine.com).