
In recent years, a variety of aggressive physical
rehabilitation programs have emerged that seem to restore significant
function for many people after spinal cord injury (SCI), even years after
injury. This article discusses several of the programs, as well as key
issues surrounding their use.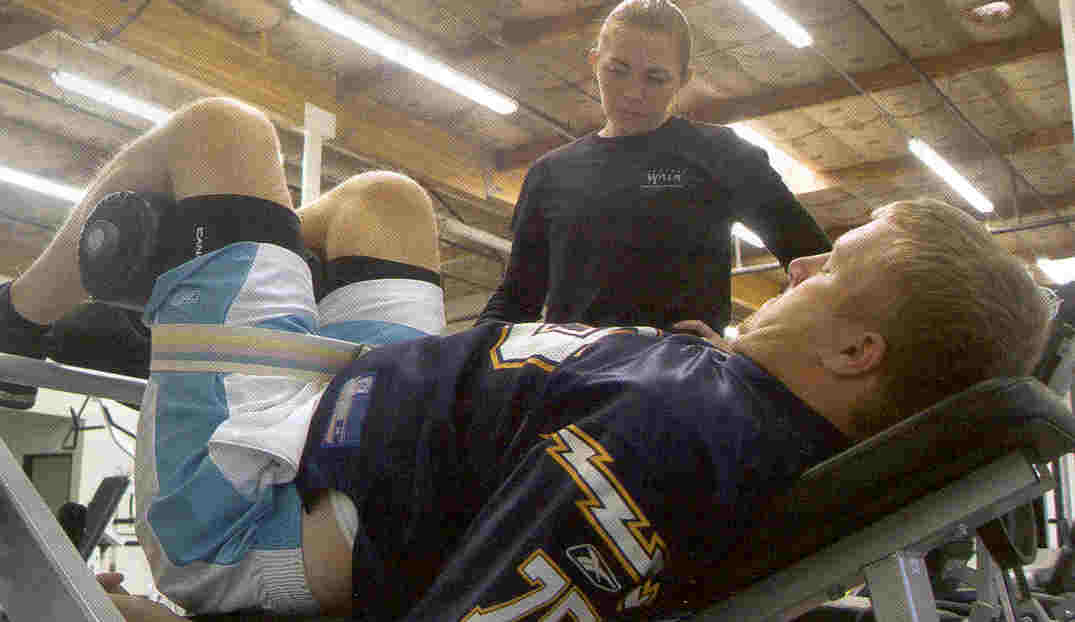
Introduction
Increasingly, such aggressive rehabilitation is being
used to maximize restored function after cell-transplantation or other
innovative surgeries that are surfacing throughout the world, including
those discussed in previous articles. Often videos are produced to
document improvement, and given the impressive nature of the physical
activities that could be done after but not before surgery, it is assumed
that the new-found abilities prove the intervention’s efficacy.
However, this assumption may not be valid; in fact,
in some cases, perhaps little of the restored function is due to the
surgery but rather to the rehabilitation aggressively pursued after
the intervention but not before. If post-surgical functional recovery
depends upon slowly regenerating neurons reaching an anatomically distant
target site, it will take a relatively long time for improvements to
appear. If during that period, the patient is enthusiastically working
out, the true cause of any ensuing improvement is questionable. As such,
some surgical interventions now require patients to aggressively
rehabilitate before, as well as after, surgery.
Furthermore, if patients believe with heart-and-soul
conviction that the surgery will help him, it will shift their
consciousness from the prior “you-will-never-walk-again” attitude that is
often imprinted on the patient’s consciousness by our medical authorities
to a self-fulfilling belief of what may be truly possible through hard
work. Their will propels them to new functional levels, perhaps only a
small amount of which is actually due to the surgery.
Even by itself, aggressive physical rehabilitation is
a complicated area in which improvements may be due to many causes and
mediating physiological mechanisms. First, such rehabilitation most likely
stimulates some function-restoring neuronal regeneration, adaptation,
and/or reconfiguration (i.e., plasticity); and also may activate dormant
but intact neurons that transverse most injury sites, even injuries
clinically classified as complete. Studies suggest that only a small
percentage of “turned-on” neurons are needed to regain significant
function.
Second, the spinal cord by itself possesses
intelligence and is not completely subservient to brain oversight.
Specifically, the spinal-cord’s “central-pattern generator” can sustain
lower-limb repetitive movement, such as walking, independent of direct
brain control. With training and braces, impressive ambulation may be
observed through physically stimulating this neural network.
Third, many muscles above the injury site indirectly
affect ambulation, especially through the use of leg braces. For example,
the latissimus dorsi (i.e., the lats), which are innervated from the
cord’s cervical region, influence pelvic-area movement and, in turn,
ambulation.
Fourth, aggressive physical rehabilitation is often
initiated in the first year after injury, a period in which appreciable
recovery potential exists. As such, critics have suggested that any
functional recovery, no matter how dramatic, would have happened anyway.
Finally, in paradigm-expanding speculations, experts
knowledgeable in Eastern and esoteric-healing traditions believe that it
is possible for brain-directed function below an anatomically complete
injury site. Specifically, a sophisticated interaction takes place between
our body’s electromagnetic energy meridians, systems, and fields and
neurological systems that can bypass the injury site. As such, it has been
suggested that martial-arts or qigong study, which emphasize energy-flow
and control, facilitates this potential.
Summaries are provided below on various aggressive,
function-restoring rehabilitation programs:
Neuro Institute
Arnie Fonseca was the driving force behind the
creation of the Neuro Institute in Tempe, Arizona (www.theneuroinstitute.com).
An exercise physiologist and former coach, Fonseca motivates clients with
SCI and other neurological disorders to regain sometimes amazing function.
I met Fonseca and was impressed with his drive, can-do spirit, and
commitment to his rehabilitation mission, which became personal after his
son Brandon sustained a serious head injury from an auto accident.
(Photo: Arnie and Cari Fonseca, with son Brandon, co-founded the Neuro
Institute)
Fonseca describes his program as immersion therapy.
He believes that the best way for a neurologically compromised patient to
get positive results is to be immersed in goal-oriented rehabilitation
therapy for at least three hours a day for 3-5 days a week. There is no
magic technique; the program uses a variety of rehabilitation approaches
ranging from electronic equipment (e.g., FES bikes) to old-fashioned,
low-tech weight training. Through his “just-do-it” motivational prowess,
Fonseca encourages patients to replace entrenched defeatist attitudes with
a new conviction of what is possible if they work hard.
Several impressive success stories are documented on
his Web site. One of the more notable involves Andrea, whose experience
represents a good example of how function-restoring surgeries are being
combined with aggressive rehabilitation. Briefly, an
omental/collagen bridge was used to bridge a 4-cm gap in Andrea’s cord
that resulted from a skiing accident (see Neurological Research 27,
2005). Since starting Fonseca’s program, Andrea regained considerable
function, including some ambulation. Time-sequential MRIs indicate ongoing
development of axonal structure through the once huge, spinal-cord gap.
Although we cannot distinguish surgical from rehabilitation contributions,
this is the sort of synergistic programs that we are going to see much
more of in the future.
Project Walk
Many people with SCI who have committed to Project
Walk (www.projectwalk.org) have accrued function much beyond what was
considered possible after injury. The intensive exercise-based recovery
program, developed by Ted and Tammy Dardzinksi in Carlsbad, California,
attempts to re-educate the damaged nervous system through physical
stimulation. Because each injured system is unique and each patient has
different capabilities, the program is tailored to individual clients.
Briefly, Project Walk focuses on developing muscle
potential below the injury level. The Dardzinksis believe standard
rehabilitation programs not only ignore this potential but contribute to
its extinction by “tossing-in-the-towel” focusing on non-paralyzed body
parts needed for adaptation to wheelchair living instead of ambulation.
They also believe the extensively administered
anti-spasticity medications are the equivalent of pouring water on the
flickering embers of regeneration that often still exist after injury. In
contrast, Project Walk’s goal is to fan these embers into a phoenix-like
reemergence of functionality.
Underscoring their reservations with prevailing
rehabilitation thinking, the Dardzinksis note: “If
you were to place an able-bodied person in a reduced gravity environment,
tell them they can’t move for a year, heavily medicate them, and give them
no hope, what do you think the outcome would be? Bone density, muscle
mass, and nervous system activity would begin to shut down and disappear.
That able-bodied person would have the same symptoms of a paralyzed
person. So, is it just the injury or the treatment that keep some SCI
paralyzed?”
Believing there is a post-injury therapeutic window
in which the recovery potential is greatest, Project Walk ideally would
like to start treating patients relatively soon after injury. The program
believes that without proper stimulation and load bearing, a newly injured
person will soon start losing bone density, muscle mass, and CNS
functioning, which makes future recovery even more difficult. Although the
program has treated many after this window, sometimes with dramatic
improvements, much more effort is needed.
Although the training schedule depends upon a
person’s function, the average client works out three hours every other
day. For people returning home, individually tailored, home-based
programs are designed. Although intensive, the program encourages clients
not to embrace it exclusively at the expense of overall life balance
achieved through involvement in areas such as career, school, social life,
etc.
The program combines strengthening activities for all
muscles in the extremities and core (abdominal, back, and pelvic), balance
work, and coordination drills. Exercises are structured to activate
paralyzed areas and strengthen weak muscles. Specialists facilitate active
and passive motions in various planes of motion to reactivate and
reorganize the nervous system. This includes floor exercises, assisted or
unassisted work on Total Gyms®, and body-weight-supported
ambulation. The common component is weight bearing through the body’s long
bones.
Functional improvements include increased muscle
mass, CNS activity, health and well being, sensation and function below
the injury level, occupational skills, and sweating, as well as decreased
drug dependence and pain.
Project Walk encourages the use of synergistic
healing modalities, including acupuncture, hyperbaric oxygen therapy,
standing frames, FES bikes, and other electrical stimulation that helps to
maintain muscle mass and circulation; and emphasizes good nutrition.
Additional aggressive physical rehabilitation
programs will be discussed in Part 2.
Adapted from article appearing in February 2006 Paraplegia News (For subscriptions,
call 602-224-0500) or go to www.pn-magazine.com).
TOP